GENERAL INFORMATION
What Is Cervical Cancer?
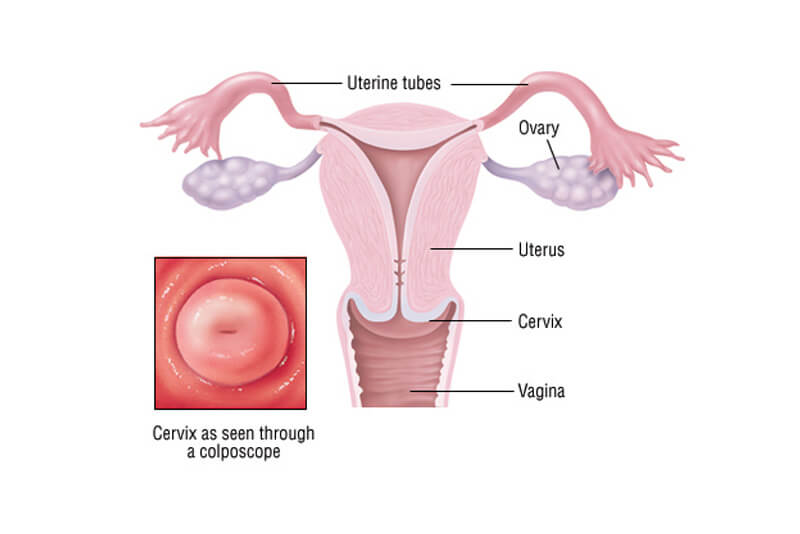
Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina.
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing most cervical cancer.
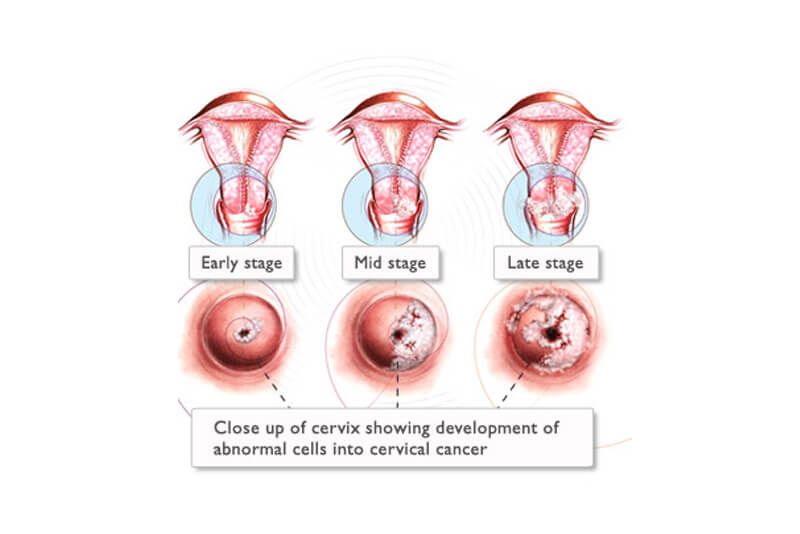
When exposed to HPV, a woman’s immune system typically prevents the virus from doing harm. In a small group of women, however, the virus survives for years, contributing to the process that causes some cells on the surface of the cervix to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.
- The part of the cervix closest to the body of the uterus is called the endocervix and is covered with glandular cells.
- The part next to the vagina is the exocervix (or ectocervix) and is covered in squamous cells.
These two cell types meet at a place called the transformation zone. The exact location of the transformation zone changes as you get older and if you give birth.
Types of cervical cancer
Cervical cancers and cervical pre-cancers are classified by how they look under a microscope. The main types of cervical cancers are squamous cell carcinoma and adenocarcinoma.
Most of the other cervical cancers are adenocarcinomas. Adenocarcinomas are cancers that develop from gland cells. Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix. Cervical adenocarcinomas seem to have become more common in the past 20 to 30 years.
Although almost all cervical cancers are either squamous cell carcinomas or adenocarcinomas, other types of cancer also can develop in the cervix. These other types, such as melanoma, sarcoma, and lymphoma, occur more commonly in other parts of the body.
SCREEN & TREAT EARLY PRE CERVICAL CANCER
Understanding Screen and Treat for pre-cancerous lesions of the cervix
Cryotherapy is extensively used to treat ectocervical premalignant lesions that occupy less than 75% of cervix and can be covered by the cryo-probe. For low- and middle-income countries (LMIC) the World Health Organization (WHO) recommends that cryotherapy be used to treat screen positive women (HPV Test or Visual Inspection with Acetic Acid (VIA)), even without colposcopic or histologic verification of disease.1
This ‘single visit approach’ will significantly increase the demand for cryotherapy in these countries. Unfortunately, cryotherapy has certain logistic disadvantages that can limit its use, such as procuring refrigerant gas, essential for the technique, or ensuring its regular supply is a major problem in many LMICs. Transporting the heavy tanks of gas is inconvenient and sometimes impossible in remote areas. The blockage of the nozzle, due to impurities, leakage of gas, etc., are other possible technical difficulties with the procedure. For this reason, it is essential to find an alternative to cryotherapy that is effective, safe, suitable and sustainable for LMICs.
Thermal coagulation™, using a portable thermalcoagulator™, destroys the transformation zone at temperatures in the 100°C to 120°C range. Thermal coagulation™ was popular in some regions (especially Scotland in the UK) in the 1970s where very high success rates were documented in several long-term studies using the Semm’s™ cold coagulation (WISAP Medical Technology™, Germany).2
The technique is as simple as cryotherapy, is an outpatient procedure, easily learned and may be performed by a range of providers including nurses. No refrigerant gas is required and multiple applications of the probe are possible to treat large lesions. In a recent review, the effectiveness of cold coagulation to treat high-grade lesions was observed to be even better than cryotherapy.3
Because there are very few recent reports of its safety and effectiveness in the published literature, and because cryotherapy predominated the practice, WHO has not included thermal ablation in its recently updated recommendations.
Liger Medical™ LLC (Liger Medical™, LLC) has developed a novel hand thermal coagulator for the treatment of cervical pre-cancers (tc thermocoagulator™), which has design advantages over the Semm’s™ cold coagulation. Briefly, it is a hand held, lightweight, inexpensive, battery operated, cordless device, which can perform approximately 50 procedures with a single fully charged battery. It is likely to be suitable for programs of cervical cancer prevention in LMICs as running electricity is not required. In vitro studies by the manufacturers suggest that it reaches the needed temperature quicker than the Semm™ coagulation (<10seconds), maintains the pre-set temperature more consistently than the Semm™ model, whilst at the same time it achieves a similar depth of destruction and does not produce smoke nor stick to the tissue post-treatment.
References:
1. WHO Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention. Geneva: World Health Organization; 2013.
2. Duncan ID. The Semm™ cold coagulation in the management of cervical intraepithelial neoplasia. Clin Obstet Gynecol 1983 Dec;26(4):996-1006.
3. Dolman L, Sauvaget C, Muwonge R, Sankaranarayanan R. Meta-analysis of the efficacy of cold coagulation as a treatment method for cervical intraepithelial neoplasia: a systematic review. BJOG 2014 Jul;121(8):929-42.